It’s with great sadness to let you know that Itzhak passed away peacefully on Jan 10, 2025 from cancer, surrounded by his family at home. We miss Itzhak dearly; you can read more about his life here.
Sinusitis Understood
This site was created by Itzhak Brook MD. It explains the diagnosis, causes, treatment and complications of sinusitis. Dr. Brook is a Professor of Pediatrics at Georgetown University Washington D.C.
Sunday, May 4, 2025
Monday, November 6, 2023
Intracranial Pyogenic Complications of Sinusitis in Children , a 20-year Study
Intracranial pyogenic complications of sinusitis in children can lead to serious sequelae. Smiljkovic and colleagues from the Hospital for Sick Children, Toronto, Canada; characterized the clinical, epidemiologic and microbiologic characteristics of children with such complications over a 20-year period.
One hundred and four cases of complicated sinusitis were
included after review. The most frequent complications were epidural empyema (n
= 50, 48%), subdural empyema (n = 46, 44%) and Pott's puffy tumor (n = 27,
26%). 52% (n = 54) underwent neurosurgery and 46% (n = 48) underwent
otolaryngological surgery. The predominant pathogen isolated from sterile site
specimens was Streptococcus anginosus (n = 40, 63%), but polymicrobial growth
was common (n = 24; 38%). The median duration of intravenous antibiotic therapy
was 51 days (IQR 42-80). Persistent neurological sequelae (or death, n = 1)
were found in 24% (n = 25) and were associated with the presence of cerebritis
and extensive disease on neuroimaging (P = 0.02 and P = 0.04, respectively).
The authors concluded that Intracranial complications of sinusitis
continue to cause significant morbidity in children. Polymicrobial aerobic anaerobic infections
are common, which reinforces the need for broad-spectrum empiric antibiotic
therapy and cautious adjustment of the antibiotic regimen based primarily on
sterile site cultures. The association of neurologic sequelae with the presence
of cerebritis and extensive intracranial involvement on neuroimaging suggest
that delayed diagnosis may be a contributor to adverse outcome.
Wednesday, June 1, 2022
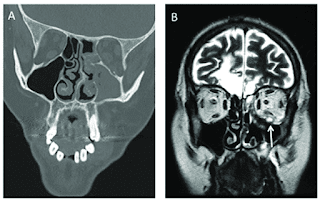
MR imaging spectrum in COVID associated Rhino-Orbito-Cerebral mucormycosis with special emphasis on intracranial disease and impact on patient prognosis
In the wake of the ongoing Coronavirus Disease 2019 (COVID-19) pandemic, a new epidemic of COVID associated mucormycosis (CAM) emerged in India.
Early diagnosis and prompt treatment of this deadly disease are of paramount importance in improving patient survival. MRI is the cornerstone of diagnosis of early extrasinus disease, particularly intracranial complications which have traditionally been associated with a high mortality rate.
Sehgal et al from Maulana Azad Medical College and Lok Nayak Hospital, New Delhi India ; presented the sinonasal, perisinus, orbital and intracranial involvement in CAM. The aim of the review is to familiarise the reader with the MR imaging spectrum of CAM with special focus on intracranial complications and a brief account of their impact on patient prognosis in the author's experience.
Special emphasis is made on intracranial disease which is categorized into vascular, parenchymal, meningeal, bony involvement and perineural spread. Vascular complications are the most common form of intracranial involvement. Some unusual yet interesting imaging findings such as nerve abscesses involving the optic, trigeminal and mandibular nerves and long segment vasculitis of the internal carotid artery extending till its cervical segment are also illustrated. In our experience, patient outcome in CAM (survival rate of 88.5%) was better compared to the pre-pandemic era. Presence of intracranial disease also did not affect prognosis as poorly as traditionally expected (survival rate of 82.8%). Involvement of brain parenchyma was the only subset of intracranial involvement that was associated with higher mortality (p value 0.016).
Saturday, January 18, 2020
Complications of Otitis Media and Sinusitis Caused by Streptococcus anginosus Group Organisms in Children.
Monday, December 25, 2017
The role of antibiotics in treating chronic rhinosinusitis.
Tuesday, September 13, 2016
Chronic sinusitis is associated with higher risk of some head and neck cancers
Saturday, September 19, 2015
Bacteriology of normal non-Inflamed sinuses and its significance
Wednesday, April 1, 2015
Clinical Practice Guidelines for Adult Sinusitis by the American Academy of Otolaryngology—Head and Neck Surgery Foundation
Monday, November 18, 2013
Chronic sinusitis may be linked to an hyperactive immune system
Tuesday, January 29, 2013
Patient’s outcome in acute invasive fungal sinusitis
Thursday, October 25, 2012
US FDA issues guidelines for developing drugs for acute bacterial sinusitis
|
The US Food and Drug Administration (FDA) has issued
guidelines for the pharmaceutical industry for developing antimicrobials for the
treatment of acute bacterial sinusitis (ABS). The FDA stated that any new drug being studied for ABS should have documenting in-vitro antibacterial activity against the most commonly pathogens associated with ABS. These include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Even though animal models of ABS has been developed, particularly for S. pneumoniae infection, they cannot substitute for clinical trials in patients that must be conducted to evaluate drug safety and efficacy. The FDA recommend that two adequate and well-controlled human trials establishing safety and efficacy be conducted for that indication. However, a single trial for an ABS indication may be appropriate if there is data from other clinical trials demonstrating effectiveness in other respiratory tract diseases such as community acquired bacterial pneumonia.
Additional supportive information like pharmacokinetic and
pharmacodynamic studies demonstrating concentration of the antibacterial drug
in the sinuses at a level expected to be active against the common pathogens
causing ABS would be required. Because direct assessment of ABS symptoms to
support a conclusion of treatment benefit in response to antibacterial drug
therapies is readily measured no surrogate markers of success of therapy are
needed.
Antimicrobials with clinically significant toxicity would not be considered appropriate for study of ABS unless treatment of a more seriously ill patient population is being considered.
|
Thursday, March 22, 2012
New guideline for the treatment of sinusitis released by the Infectious Diseases Society of America (IDSA).
Wednesday, February 15, 2012
Is amoxacillin an adequate agent for the treatment of sinusitis?
Saturday, December 17, 2011
Are systemic corticosteroids effective in relieving symptoms of acute sinusitis?
Wednesday, April 13, 2011
Is there a link between acid reflux and chronic sinusitis?
Acid reflux into the oesophagus, larynx, pharynx or nasopharynx has been suggested as a causal factor in chronic rhino-sinusitis (CRS ), which can then be refractory to nasal treatments. A recent review by Flook & Kumar (Rhinology 2011) evaluated the strength of the link between acid reflux and nasal symptoms and CRS .CRS patients. Paediatric cohort studies showed more reflux events in rhinosinusitis patients than the general paediatric population, but they are not conclusive. Many of the papers did not use robust CRS diagnostic criteria for inclusion into studies and take no confounding factors into consideration.CRS and there is no evidence that acid reflux is a significant causal factor in CRS .
Wednesday, March 23, 2011
Increase in the Frequency of Recovery of Methicillin Resistant Staphylococcus aureus (MRSA) in Acute and Chronic Maxillary Sinusitis
Wednesday, December 22, 2010
Sinusitis after radiation is caused by resistant bacteria
Monday, December 20, 2010
Are Topical Antibiotic Effective in Treating Chronic Sinusitis?
Topical antibiotic delivery devices to date have included nasal sprays, irrigations, and nebulizers. Nasal spraying of topical antibiotics are not believed to be very effective. This is supported by studies that have shown that the majority of deposition occurs only in the anterior part of the nasal cavity. In addition, the nasal sprays rely on mucociliary clearance to transport the drug from the anterior to the posterior nasal cavity, and in patients with CS, their mucociliary clearance may be impaired. There are, however, other studies that found nebulization and irrigation to be effective.
Fungi can play a role in the pathogenesis of CS both in an allergic and inflammatory manner. Several recent studies that evaluated the efficacy of topical amphotericin B showed trends that were promising. However, most of the placebo-controlled studies showed no statistical difference between the treated patients and untreated controls.
Recent animal studies found that mupirocin was effective in reducing Staphylococcus biofilm mass by over 90%. Staphylococcus aureus-related acute exacerbations of chronic sinusitis in patients was also treated effectively with topical mupiricin. No success was, however, achieved with aminoglycosides in reducing Pseudomonas aeruginosa biofilm.
Since most of the initial clinical work done with topical antibiotics in CS was retrospective, prospective studies are warranted to further evaluate the utility of this approach. These should evaluate the efficacy of antimicrobials, antifungals and steroids alone and in combinations.
Sunday, December 19, 2010
Smoking and sinusitis
In a recent study we evaluated the microbiology of sinus aspirates of smokers and nonsmokers with acute (244 patients, 87 smokers and 157 nonsmokers ) and chronic (214 patients, 84 smokers and 130 nonsmokers) maxillary sinusitis. We found that sinusitis in smokers is more often caused by antibiotic resistant bacteria including methicillin resistant Staphylococcus aureus (MRSA) than in non smokers.
Oropharyngeal ccolonization with potential bacterial pathogens is higher in smokers than non smokers. Cesation of smoking reverses the increased colonozation by pathogens.